HPV and Anal Cancer
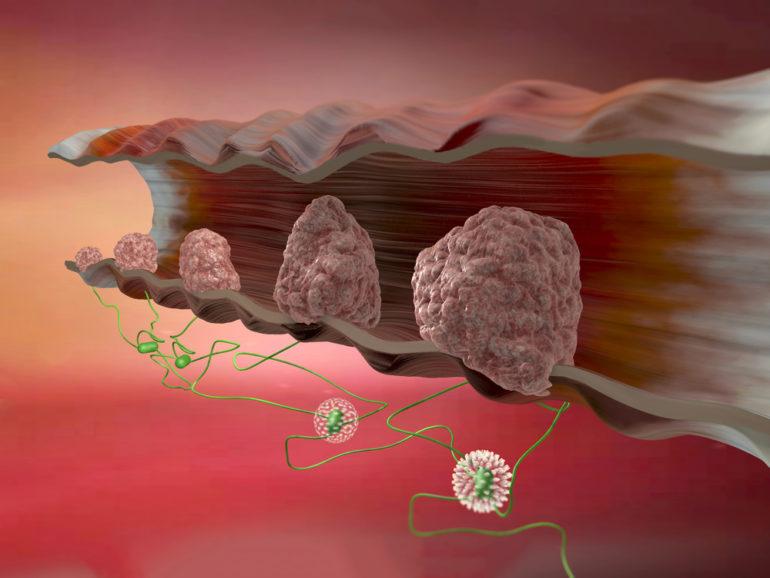
Anal canal is the name given to the last part of the intestine/large intestine. Anal cancer is mostly squamous cell cancer originating from cell layer (epithelium) spreading inside of the anal canal. Anal cancer creates 2.2% of stomach intestinal cancer.
The studies performed in the last 20 years demonstrate that there is close relationship between anal cancers and HPV infection. On the other hand, anatomic structure of anal canal exactly resembles cervix and there is a transition zone in the cervix similar to the cervical canal. Both the role of HPV in terms of development of anal cancer and similarity between anal canal and cervical canal cause anal cancer to be included in preventable diseases class such as exactly the cervical cancer.
Although anal cancer is one of rarely encountered cancers, its frequency increases 2% every year. While anal cancer was observed more frequently in females in the past, the difference related to the frequency between males and females gradually decreases. Especially anal cancer precursor lesions are observed approximately in the same frequency at the moment in terms of the females and males. While anal cancer is observed in older ages in females (60-65 age), it is observed in younger ages in males (40-45 age).
Anal cancer precursors and the relation between anal cancer and HPV infections
HPV infection is detected in 71% of anal cancers and especially in 78% of squamous cell cancers. HPV type 16 is positive in a large part (85%) of the patients with HPV positive. HPV type 18 (7%), 33, 31 and 45 is detected in a lesser part. While HPV positivity is (91%) in high graded anal cancer precursor lesions (H-ASIL), it is 88% in low graded ones (L-ASIL). Low graded anal cancer precursor lesions are especially related to HPV Type 6, 11 (low risk HPV). American Disease Prevention Office notifies that 93% of anal cancers is associated with HPV infection.
Risk factors of anal cancer precursor lesions and anal cancer related to HPV infection:
*Anal HPV infection
*Females previously having disease relevant to HPV in cervix or vulva.
*The ones previously having cancer relevant to HPV
*High risk sexual affairs (having anal intercourse passively)
*HIV infection *Patients, whose immune system is suppressed chronically
HPV DNA is detected in large part of the anal cancers and anal cancer precursor lesions. High rish group in the researches made about the subject is homosexual patient groups, who are having anal intercourse without protection, and HIV positive patients. HPV Type 53, 58, 61 and 70 are frequently encountered in anal canal of the ones, who are having homosexual intercourses. These HPVs are medium-high risk HPV. Isolating HPV Type 32, which is an oral type, from anus suggests that HPV may be infected by oral-anal intercourse. Detection of HPV 31,33 and 35 detected in the ones, who had anal wart, in oral samples also marks in another study that HPV may be infected by anal-oral intercourse.
Although no difference is observed in terms of HPV type between HIV (+) individuals and (-) individuals, it is known that more HPV type is encountered in the ones, who have HIV (+).
Having cervix cancer previously also increases anal cancer risk. This also reveals the effectiveness of HPV on anal cancers.
Development and Prognosis (Course) of Disease in Anal Cancer Related To HPV
The relationship between anal cancer precursor lesions and anal cancer resembles the relationship between cervical cancer precursors (CIN) and cervical cancer.
Anal cancer precursor lesions are also divided into 2 as high grade (HGAIN) and low grade (LGAIN) just like cervical cancer precursors in other words cervical dysplasia (CIN I, CIN II, CIN III). Although a part of low grade anal cancer precursor lesions regress automatically, it is predicted that a part of them is directed to change towards cancer. 9-13% of high grade lesions transform into anal cancer.
HPV also in anal cancer causes development of cellular immortality by repressing P53 and Rb genes over E6 and E7 proteins and transformation of these cells into cancer by being reproduced uncontrolledly like in cervical and head and neck cancers.
Clinical Characteristics In the Context Of HPV Infection In Anal Cancer
Squamocolumnar junction included in anal canal (transition zone of 2 different cell types) resembles very much to transition zone in cervical canal. This region is the area, which is infected by HPV, thus anal cancer occurs as in cervix. HPV infection occurs in 3 ways in anal canal; Latent infection: There is HPV but no cellular change or lesion occurs. Subclinical HPV infection: There are AIN (anal carcinoma lesion, in which in situ-cancer cells do not pass bottom layer) or similar lesions in HPV anal transition zone, it is noticed by the investigations. Clinical infection: anal wart or anal cancer occurs.
85% of anal cancers is squamous cells and HPV infection is related to this group.
Screening is recommended for AIN (anal carcinoma lesion, in which in situ-cancer cells do not pass bottom layer).
Screening is performed by receiving smear just like in cervical screening program. However, cotton buds are used as it will be received from anal canal. The problem is that the effectiveness of anal cancer screening programs is not proved for the population under risk. Deaths definitely reduce by smear in terms of cervical cancer and while early diagnosis is made perfectly, this efficiency of swabs received from anal canal could not be demonstrated clearly. Correspondingly there is no consensus belonging to by which method the screening strategies and results will be treated.
But it is still the single option we have and it should absolutely be made especially in risky population (on the one, who has anogenital wart, patient with HIV positive, homosexual patients, the ones with multi-partners or having risky sexual acts).
PROGNOSIS (Course of Illness)
The studies specifying the course of the diseases of HPV (+) anal cancer patients compared to HPV (-) patients are insufficient. Yes, there is a relation between HPV and anal cancer and it is efficient; however, it is not clearly known how much it would affect the course of cancer.
HPV Vaccines and Anal Cancer
6In prospective randomized study performed on 602 homosexual males, HPV vaccines of 4 are demonstrated to decrease development frequency of high grade anal intraepithelial neoplasia (AIN) at 54% rate in sexual active cases. This is quite important. The vaccine provides protection at a certain rate even though the person is sexually active.
Reference
Leszczyszyn J, Łebski L, Łysenko L et al. Anal warts (condylomata acuminata) – current issues and treatment modalities. Adv Clin Exp Med. 2014 Mar-Apr;23(2):307-311.
Nyitray AG, Carvalho da Silva RJ, Baggio ML et al. Age-specific prevalence of and risk factors for anal human papillomavirus (HPV) among men who have sex with women and men who have sex with men: the HPV in men (HIM) study. J Infect Dis. 2011 Jan 1;203(1):49-57
Shvetsov YB, Hernandez BY, McDuffie K et al. Duration and clearance of anal human papillomavirus (HPV) infection among women: the Hawaii HPV cohort study. Clin Infect Dis. 2009 Mar 1;48(5):536-546.
Kofoed K1, Sand C, Forslund O, Madsen K. Prevalence of human papillomavirus in anal and oral sites among patients with genital warts. Acta Derm Venereol. 2014; 94(2):207-211.
Weis SE. Current treatment options for management of anal intraepithelial neoplasia. Onco Targets Ther. 2013; 10: 651-665.
Assoumou SA, Panther LA, Feng Y et al. Treatment of high-grade anal dysplasia in high-risk patients: outcome at an urban community health centre. Int J STD AIDS. 2013; 24(2):134-138.
Poggio JL. Premalignant lesions of the anal canal and squamous cell carcinoma of the anal canal. Clin Colon Rectal Surg. 2011; 24:177-192.
Palefsky JM, Giuliano AR, Goldstone S et al. HPV vaccine against anal HPV infection and anal intraepithelial neoplasia. N Engl J Med. 2011; 365(17):1576-1585.
2 Ağustos 2016 tarihinde Prof. Dr. Süleyman Engin Akhan tarafından yayınlanmış ve 20 Kasım 2018 tarihinde de son güncelleme yapılmıştır.