Treatment Principles in Cervical Cancer and Stage IA Cervix Cancer Treatment
Cervical Cancer treatment is planned according to the child wish, general condition and stage of the patient.
Especially in some certain conditions about which I shall give some details later on, it is important that the treatment options are decided by the gynecologic oncology council. The benefits of the council are both that a decision is made with a joint intelligence and that the responsibility of a long running process of the oncological treatment is not undertaken by one person. Because there can always be problems faced during the process. (In the gyneco-oncology council; there are gyneco-oncologists, medical oncologists, radiation oncologist, gyneco-pathologists and radiologists expert in gynecologic tumors.)
Surgery is sufficient for early stage cervical cancer treatment, while when the general condition of the patient is not fitting, i.e. the patient cannot receive anesthesia, radiotherapy can be used.
. In the treatment of the advanced stage cervical cancer usually chemotherapy and when necessary surgery is applied.
You will see the treatment of cervical cancer based on its stages below. First of all it should be stressed that the thing written here are only treatment schemes recommended in the frame of certain international and national directives. So they are just recommendations in any case. Each patient is special in its condition. The phrase “there are no illnesses, there are patients” is especially true for the oncology patients. In some cases the method needed to be applied for therapy is clear as surgery or chemo-radiotherapy or both and sometimes it is very intricate. At the end, the things you read here are just recommendations 😊
The treatment schemes you may see below are shaped under the scope of NCCN Guidelines Version 1.2017 Cervical Cancer (https://www.nccn.org/professionals/physician_gls/f_guidelines.asp), ESMO Cervical Cancer Guideline 2017 (http://www.esmo.org/Guidelines/Gynaecological-Cancers/Cervical-Cancer) and the directives published by the Gynecological Oncology Algorithm Group (Gynecological Tumors, Diagnosis-Treatment-Follow up, Cervical Cancers. Ed: A.Aydıner, I.Aslay, S.Berkman. Nobel Tıp Kitapevi. 2016: 123-169 (http://tukod.org/folders/file/WWeb_JT_2016(1).pdf).
I-Stage 0 and Stage I Cervical Cancer Treatment:
Stage 0 and I cervical cancer is a very early stage, the tumor is limited within the cervix.
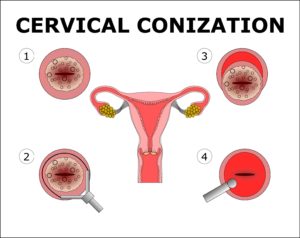
Thus it is possible to protect the fertility of the patient. Therefore the age and desire to protect fertility of the patient shapes the treatment. However, first of all for the diagnosis, i.e. to understand whether it is stage IA1 or not, conization should be done and the properly performed conization both provides the understanding of how deep the invasion of the cancer is present in the tissue and performs the treatment.
I tried to explain for many times before but I shall explain again. If you spare time and carefully look at the staging steps above you can see there is a millimeter difference between Stage IA1 and IA2. The difference can be millimetric but it is really important regarding the surgery to be made. In Stage IA1 a simple womb removal surgery is sufficient whereas in Stage IA2 radical surgery, even pelvic lymph nodes removal (pelvic lymphadenectomy) are added to this. Several millimeters cause this much difference.
You can see the relation between tumor invasion and basal layer. Abnormal cells need to pass the basal layer that then cervical cancer is an issue.
Thus a straightforward mentality of “Why they are performing two surgeries to me, why does not it end in a single time” is not proper my friends 😊
Another point is also very important! What we talk about here is “Invasive cancer” and its treatment. It is not CIN II (CIN 2) or CIN III (CIN 3) or HGSIL, ASC-H treatment. Do not confuse them. For example, CIN 3 is detected in biopsy and conization is performed; the margin is positive but there is no “invasion” then the method is different, if you have Stage IA1 invasive cervical cancer and the margins came back positive, then the method is different. Please do not confuse them and panic unnecessarily.
In Stage IA1 3 fundamental points are important:
1. Does patient want to protect fertility?
2. Is the patient in a condition proper for surgery?
3. Is there a lymphovascular invasion (LVAI)? I have given in detail above but it is necessary to write once again; lymphovascular invasion means that there are cancer cells seen between capillaries and lymph ducts around the tumor.
After the answers of these questions are assessed by the surgeon the treatment is shaped. Frankly, in this stage radiotherapy is a treatment option for old patients and patients with medical problems.
In Stage IA1 we definitely can cure the patient without removing the womb and while protecting the fertility. In the case with negative surgical margins and negative sampling from endocervical canal (ECC), conization completes the treatment of the illness.
Because lymph node metastasis rate in this group of patients is 0.8% and lower.
The most important property of the conization is that it allows the removal of the ectocervix and endocervical canal covering the transformation zone. In an experienced hand complication rate is very low.
In the NCCN 2017 cervical cancer guide it is suggested that “cold conization” with a scalpel should be preferred, however the use of this method is gradually decreasing because both complication frequency is high and it affects the fertility more negatively compared to the LEEP cornization. You can find detailed information on the subject on the site.
After the post cornization invasion depth is determined clearly and if the patient wants to protect her fertility conception, if she does not then removal of the womb by Type I (Simple) Hysterectomy can be recommended.
In order to ensure that the conization has completed the treatment:
1. After the operation 2 endocervical curettage (ECC=biopsy taken from womb canal) results should be negative.
2. Lymphovascular invasion (LVAI) should not be present. If LVAI is present the recurrence rate of the tumor increases from 3.2% to 9.7%.
3. Surgical margin should be negative. If the margin is positive it is reported that the possibility of the patient having lesion going deeper than 3 mm, i.e. that is Stage IA2, is 10%.
When these criteria are met, i.e. ECC and surgical margin are negative, and LVAI is not present then the recurrence risk of the illness is reported as less than 0.5% (Benedetti-Panici P. Cancer 2000; 88:2267-2274)
). However in case of lymphovascular invasion or the surgical margins in the conization are positive then the situation changes.
If the margins are positive in conization there are 2 options to apply, where I prefer the first one. My preference is to repeat conization. This gives us the real invasion depth of the tumor. If the invasion is still at Stage IA1 level then the patient is monitored. Whereas the second option is to perform “trachelectomy”.
Trachelectomy means the removal of the cervix completely as to include the upper 1/3 section of the vagina, the ligaments carrying the womb and the most importantly the tissues by the cervix called parametrium for protecting the fertility in the selected invasive cervical cancer cases. Thus only the body of the womb is protected.
Gastric type cervical adenocarcinoma and adenoma malignum are 2 types of cells that trachelectomy should not performed on.
Despite it is an aggressive surgery, it is a perfect surgery applied to protect fertility in especially Stage IA2 and Stage IBI-2 cases.
As a result, in Stage IA1 cervical cancer patients, if no LVAI is present, if the patient wants to protect the fertility, as long as the margins are negative the conization is the sufficient treatment. In women whose fertility ended, normal (extrafacial=Type I) hysterectomy completes the treatment.
. In the patient group treated with conization, after the fertility is ended, if there are repeating HPV infection or abnormal pap-smear results are present in the controls, simple hysterectomy performance is recommended in these patients.
In the patients with LVAI, the possible risks are shared with the patient, and in case the pelvic lymph nodes are removed and there is no metastasis in the lymph nodes and the surgical margins of the cornization material are negative, the pregnancy is permitted under close monitoring.
In the cornization material if the margins are positive, according to the preference of the gynecologist oncologist, for well assessment of the invasion degree to be made, re-cornization or radical trachelectomy should be made.
3 Eylül 2017 tarihinde Prof. Dr. Süleyman Engin Akhan tarafından yayınlanmış ve 16 Kasım 2018 tarihinde de son güncelleme yapılmıştır.