Stage IA2 and Stage IB / IIA1 Cervical Cancer Treatment
First of all it is better to emphasize again that The treatment schemes you may see below are shaped under the scope of NCCN Guidelines Version 1.2017 Cervical Cancer (https://www.nccn.org/professionals/physician_gls/f_guidelines.asp), ESMO Cervical Cancer Guideline 2017 (http://www.esmo.org/Guidelines/Gynaecological-Cancers/Cervical-Cancer) and the directives published by the Gynecological Oncology Algorithm Group (Gynecological Tumors, Diagnosis-Treatment-Follow up, Cervical Cancers. Ed: A.Aydıner, I.Aslay, S.Berkman. Nobel Tıp Kitapevi. 2016: 123-169) (http://tukod.org/folders/file/WWeb_JT_2016(1).pdf). Before reading this section looking at the Cervical Cancer Staging section shall help you understand the issue better.
Stage IA2 Cervical Cancer Treatment
In Stage IA2 the stromal invasion (spreading of the tumor down from the basal layer) measured is about 3.0mm to 5 mm. And at this invasion depth the possibility of the tumor to reach to lymph nodes is high. Thus the standard treatment of the Stage IA2 cervical cancer is:
Uyarı: +18 Doğrulama Gerekmektedir.
Görüntülemeye çalıştığınız içerik/görsel +18 doğrulama gerektirmektedir.
Eğer 18 yaş ve üzeri olduğunuzu doğruluyorsanız "e-posta" sekmesine
e-posta adresinizi yazarak, "Doğrula" butonuna tıklayınız.
I) Modified radical hysterectomy (Type B) and pelvic lymphadenectomy on both sides or if the medical condition of the patient prevents surgery or the patient does not want it then II) Radiotherapy.
Both treatment ways, whether the patient receives a surgery or radiotherapy, have the same survival periods. The difference is the complications developed depending on the treatment ways.
Stage IB and IIA1 Cervical Cancer Treatment
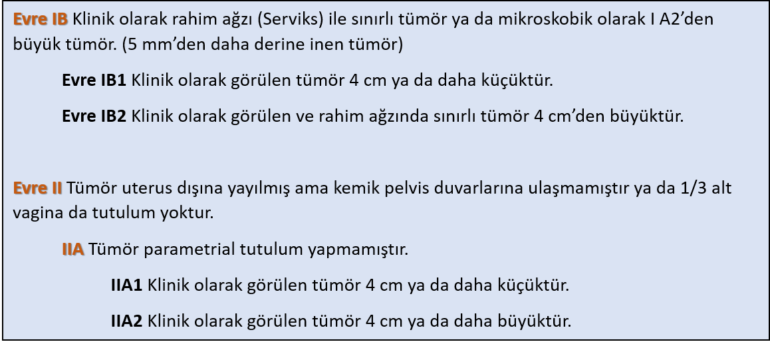
As seen above at Stage IB tumor is limited at the cervix. Whether it is bigger than 4 cm is important regarding the treatment to be applied.
If you refer to the classical book information, for example NCCN states that the treatment in Stage IB –IIA patients can be done via Surgery and Chemo-radiotherapy. ESMO indicates that it can be treated surgically or through chemo-radiotherapy and both treatments are equivalent regarding survival and the difference is the complications that may occur.
The standard approach in surgery is “Radical Hysterectomy (Type III) + Pelvic and Paraaortic lymphadenectomy”.
However there are problems that occur during practical applications.
Whether on Stage IB or Stage IA1/2, if the tumor is bigger than 4 cm the possibility of the patient to receive radiotherapy or chemotherapy as an additional treatment after the surgery increases.
This condition also increases complication frequency. The ideal is that the patient only goes under surgery or only receives chemo-radiotherapy. The reason is that during Type III Radical Hysterectomy we remove largely the tissues we call parametrium where the cervical cancer usually spreads, i.e. the womb and neighboring tissue, ligaments.
If subsequently it become mandatory to give the patient radiotherapy, and we frequently do, then the complication risk increases. Thus the ideal is to apply either surgery or chemo-radiotherapy. Surely, even we are extremely careful in assessment and check with sophisticated imaging methods, at the end both treatments are needed to be applied in some patients but it is better that we lower this ratio as much as we can.
There is only and only one academic research that evaluated both treatment options as prospective randomized way: “Landoni F, Maneo A, Colombo A et al. Randomised study of radical surgery versus radiotherapy for stage IB-IIA cervical cancer. Lancet 1997; 350: 535–540.”
As you can see Landoni et. al. published it all the way back in 1997. Well why no other studies performed since then, I can hear you saying sit down and do it brother, but it is incredibly hard to perform such studies. On one side it is hard ethically. Let us keep on the point but it is really hard my friends.
Uyarı: +18 Doğrulama Gerekmektedir.
Görüntülemeye çalıştığınız içerik/görsel +18 doğrulama gerektirmektedir.
Eğer 18 yaş ve üzeri olduğunuzu doğruluyorsanız "e-posta" sekmesine
e-posta adresinizi yazarak, "Doğrula" butonuna tıklayınız.
Well, what is the result of the study? Landoni et. al. have evaluated 343 cervical cancer patients in Stage IB-IIA. And 5 year survival rates were same in both groups. Meaning, whether the patient received surgery or radiotherapy at the end of 5 years the rate of the surviving patients is same, where the number is very high. However 66% of the women who received surgery also needed to receive additional radiotherapy.
But the most important thing is that the severe complication risk in the surgery group as they received additional radiotherapy was much higher than the only radiotherapy group, more than two folds (28% surgery group, 12% only radiotherapy group)!
Thus we do not like much the case of let us operate then we can give radiotherapy anyway. It increases our complication risk and some of them are really severe.
Now it is time for the question of how we select the patient. When selecting patients we look at primary to the age, weight, tumor volume and whether the patient is sexually active. According to these criteria the treatment process is determined but the most important thing is to the take this decision via talking to the patient and her family. The patient and her kin should know which treatment we choose and not the other.
In 2014 a group of gynecologist oncologists from South Korea published and algorithm to be used in treatment selection of Stage IB-IIA patients. According to this they divided the patients into 4 groups and called it “4 Factor Model”: Tumor diameter over 3 cm, deep stromal invasion at the outer side of the cervix (i.e. tumor going deep), LAVI detection, cell type being adenocarcinoma or adenosquamous cancer. They said that if 2 of these 4 risk factors are positive then the tumor reoccurrence possibility is very high after a Type III womb removal surgery and you should conduct your treatment accordingly.
Such classifications are continuously done and they are no other than evaluation of known risk factor however the problem is at the foundation of the science and it is shaped in a cliché wording: “There are no illnesses, there are patients.” Thus we need to shape the treatment considering all the risk factors we listed and according to the patient.
Cancer treatment is a long running treatment. When the family is informed on the risks and possibilities in detail and clearly at the very beginning, then if a complication occurs during the process, it is easier to fight.
However one point should be stressed over and over again. I am not going into much detail here but there are also different approaches. For example NCCN directives suggest that during Stage IB2 and Stage IIA2 cases chemotherapy should be applied right after radiotherapy. Again some people attending the NCCN panel advocate that in Stage IB-IIA cases, after pelvic lymphadenectomy, if lymph nodes are negative and tumor is not present the surgery should continue.
Can fertility be protected at Stage IB1?
Yes this can be achieved. However in a very limited patient group. Well what we do? Radical trachelectomy + Pelvic and (according to the surgeon’s choice) Paraaortic lymphadenectomy is applied and the fertility can be protected. If the tumor is under 2 cm this method works. Meaning, it is not sufficient to be at Stage IB1, in addition the tumor diameter should be maximum 2 cm. In larger tumors, controlling spreading and relapse is very hard.
3 Eylül 2017 tarihinde Prof. Dr. Süleyman Engin Akhan tarafından yayınlanmış ve 16 Kasım 2018 tarihinde de son güncelleme yapılmıştır.